Introduction
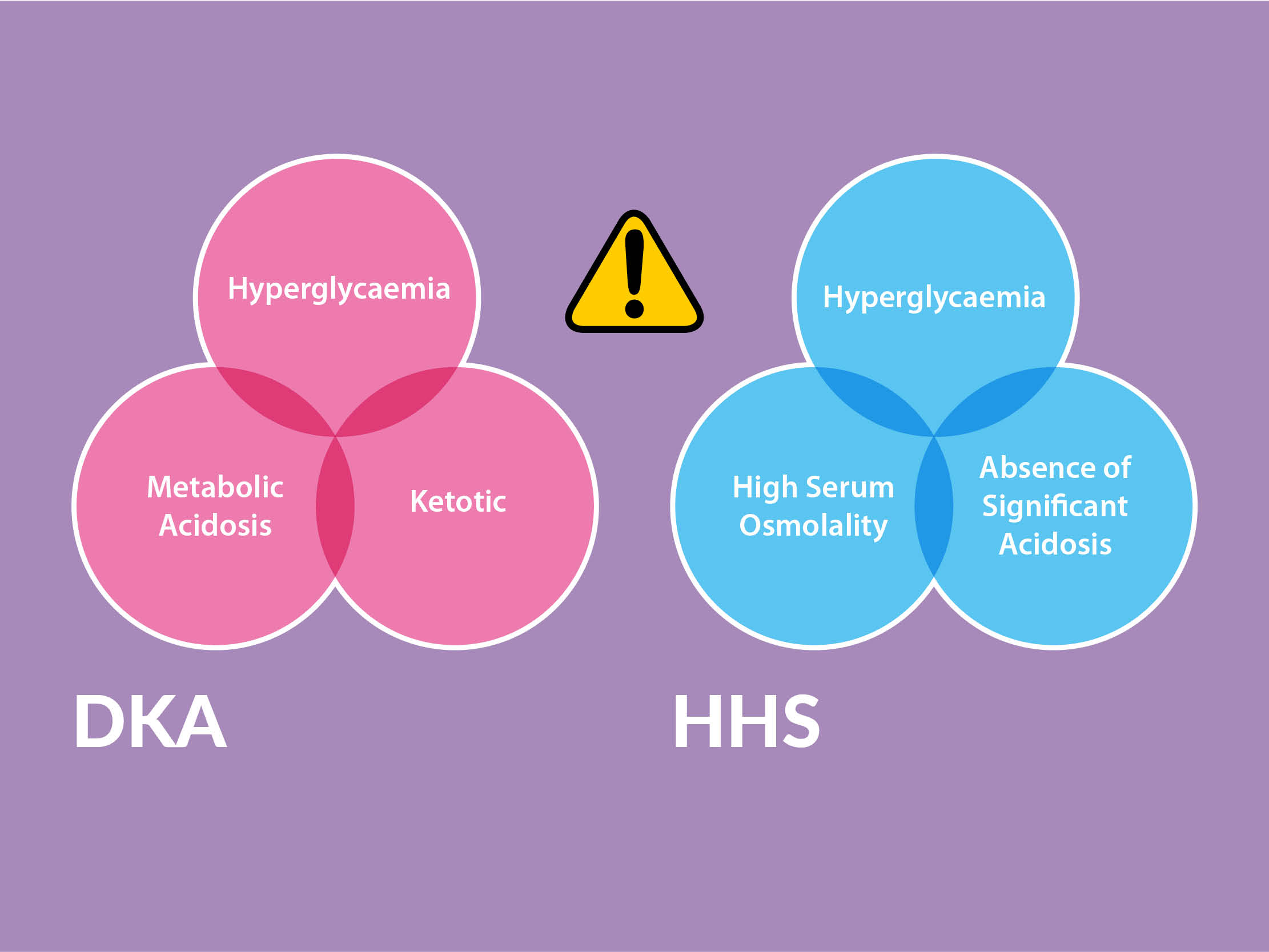
This section gives guidance and links to guidelines on the management of diabetes emergencies, diabetic ketoacidosis (DKA) and hyperosmolar hyperglycaemic state (HHS) in adult patients. This section also provides guidance and information on managing unwell patients with diabetes who are not in DKA or HHS.
Diabetic Ketoacidosis (DKA) is an emergency which mainly occurs in patients with type 1 diabetes
DKA definition and management:
Significant ketonuria (≥ 2+) or blood ketone > 3mmol/L
Blood glucose > 11mmol/L or known diabetes mellitus
Bicarbonate < 15mmol/L or venous pH < 7.3
Insulin: commence Fixed Rate Intravenous Insulin infusion (FRIII) as soon as diagnosis of diabetic ketoacidosis (DKA) is confirmed
Fluid: replace fluid deficit, follow protocol and take care in adolescents/young adults and elderly due to the risk of fluid overload or cerebral oedema
Potassium: monitor hourly initially and replace potassium according to protocol to avoid hypokalaemia which can occur as complication of treatment
Avoid hypoglycaemia: monitor capillary blood glucose (CBG) hourly and when CBG <14mmol/l start iv dextrose according to protocol
Identify and treat any underlying cause
NOTE: DKA requires prompt active management, early senior review and hourly assessment. It is important to avoid hypokalaemia, hypoglycaemia and fluid overload by meticulous clinical review and adherence to the guidelines. Involve the specialist diabetes team early. Use a DKA proforma if available in your hospital.
Links:
ITS ANIMATION: FRIII to SC
Hyperosmolar Hyperglycaemic State (HHS) which occurs in patients with type 2 diabetes
HHS definition:
Hypovolaemia
Marked hyperglycaemia (≥30 mmol/L) without significantly elevated blood ketone levels (<3 mmol/L) or acidosis (pH>7.3, bicarbonate >15 mmol/L)
Osmolality ≥320 mosmol/kg (2Na + Gluc + Ur)
Insulin: commence Fixed Rate Intravenous Insulin infusion FRIII* if diagnosis of hyperglycaemic hyperosmolar syndrome (HHS) is confirmed.
Fluid: follow protocol – caution in the frail elderly due to risk of fluid overload
Potassium: monitor and replace according to protocol
Low molecular weight heparin – prophylactic regime
Identify and treat underlying cause
Mortality associated with HHS is high, senior review and active management are required. Involve the specialist diabetes team early – many of these patients will require insulin treatment.
NOTE: *Insulin FRIII dosing and iv fluid regime is different for HHS compared to DKA. Ensure you are following the right management protocol.
Links:
Acutely unwell patient with diabetes, not in DKA/HHS
The majority of medical patients with diabetes (Type 1 and Type 2) who are hyperglycaemic, well, able to eat and drink and are not in DKA/HSS can be managed without iv insulin (variable rate intravenous insulin infusion (sliding scale) – VRIII).
Use variable rate intravenous insulin infusion (VRIII) for patients with known diabetes if they are acutely unwell (DKA/HHS excluded) / unable to take oral fluid/food / requiring rapid control of CBG / remain persistently hyperglycaemic following 2 consecutive PRN doses of Novorapid (see Hyperglycaemia decision support tool)
For further guidance on indications for use of VRIII in medically unwell patients see links below or go to chapter on VRIII. Guidance also includes advice on iv fluid choice and safe transfer to S/C insulin.
Links:
• Adult UHL Hyperglycaemia decision support tool
• Adult UHL Insulin dose titration decision support tool
• Adult national guidance – VRIII - JBDS
If unsure ask for help either from diabetes team or a senior doctor.